Thunder Bay Police Service
For first responders, trauma is a regular workplace hazard. As a result, people working in these fields are disproportionally affected by mental health issues.
Mental illness affects nearly 10 per cent of Canadians, but more than 36 per cent of Canadian police officers. Research by the Centre for Addiction and Mental Health took a deeper look at the issue in 2018 and found just how severe the impact is on frontline officers.
Nearly 90 per cent of officers participating in the CAMH study reported moderate to severe levels of depression, with 13 per cent experiencing severe depression. Meanwhile, almost a third of officers surveyed showed signs of being in the clinical diagnostic range for post-traumatic stress disorder.
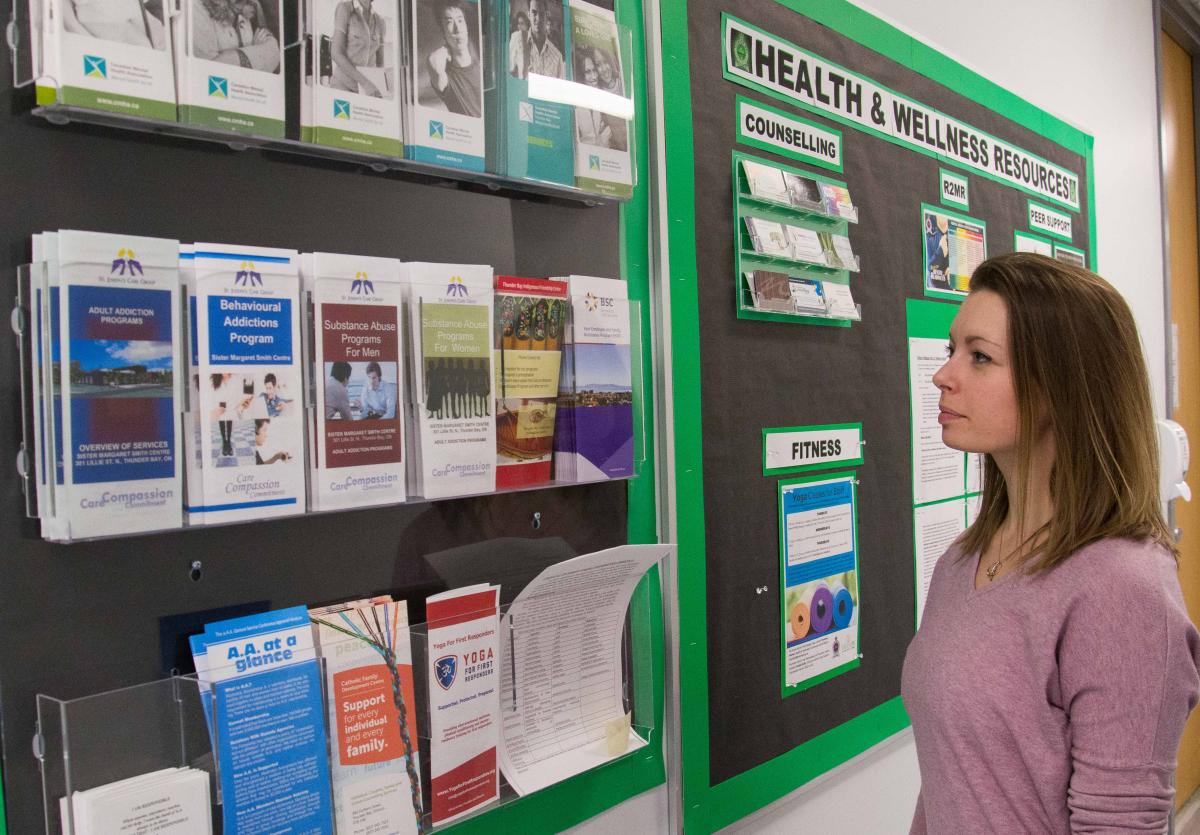
Cst. Gerald Duffy is the Thunder Bay Police Service’s Critical Incident and Peer Support Coordinator. He, and the 22 volunteer members of the peer support team, are working to address these mental health issues.
“We’re not psychologists,” Cst. Duffy says of the peers support team members. “We are a caring ear, a compassionate person who has been through what you’ve been through and can relate. We’re a non-judgmental and confidential person that a lot of people need.”
The Thunder Bay Police Service’s peer support team formed three years ago as the result of growing nation-wide demand to have such services available to first responders. Cst. Duffy was a volunteer member of the team since its inception, and became the coordinator in April 2018. The position was previously held by S/Sgt. Jeremy Pearson and then Sgt. Michael Tomasevic.
The other 22 members are sworn and civilian Thunder Bay Police Service employees who are part of the team voluntarily.
“They do this work in addition to their regular duties,” Cst. Duffy says, “and they make themselves available to members in need.”
 The availability is key, as a critical incident -- such as an incident involving the death of a child, or significant injury or death of a member -- can take place at any time.
The availability is key, as a critical incident -- such as an incident involving the death of a child, or significant injury or death of a member -- can take place at any time.
When a critical incident does occur, Cst. Duffy works with available peer support members and clinical psychologist Dr. Sara Hagstrom to develop a strategy to meet with affected members before they leave at the end of their shift.
After that, the peer support team works toward having a complete debriefing within 72 hours of the incident.
“It’s been proven that doing these formal debriefings lessens the negative effects to the individual,” Cst. Duffy says. “In the past a critical incident would have occurred and the member would go home and try to cope by themselves and may have then fallen into alcoholism, insomnia, high blood pressure, or worse.”
Stigma remains an uphill battle for the peer support team. Fear that asking for help might be seen as a sign of weakness is still an issue, and one that could lead members to go it alone after traumatic incidents.
Nevertheless, Cst. Duffy believes the work of the peer support team is pushing back against this stigma.
“It is changing,” he says. “People are more open to asking for help and not seeing it as a sign of weakness. I think it’s comforting to know that you have someone, a group of individuals, who are taking this seriously, staying confidential and showing that they care.”
Jan. 30 is Bell Let’s Talk. On Bell Let’s Talk Day, Bell will donate five cents for every applicable text, call, tweet or social media video view and use of their Facebook frame or Snapchat filter. Learn more at : letstalk.bell.ca